Abstract
Background:
Medicare reimbursement cuts have been associated with declining gonadotropin-releasing hormone (GnRH) agonist overuse in localized prostate cancer. Medical school affiliation and foreign training have been associated with persistent overuse. However, physician-level prescribing changes and the practice type of persistent overusers have not been examined. We sought to describe physician-level changes in GnRH agonist overuse and test the association of time in practice and solo practice type with GnRH agonist overuse.
Methods:
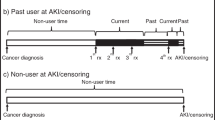
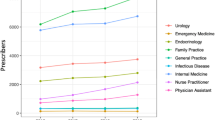
We matched American Medical Association physician data for 2138 urologists to Surveillance, Epidemiology and End Result-Medicare data for 12 943 men diagnosed with early-stage and lower-grade adenocarcinoma of the prostate between 2000 and 2007. We conducted a population-based, retrospective study using multilevel modeling to control for patient and provider characteristics.
Results:
Three distinct patterns of GnRH agonist overuse were observed. Urologists’ time in practice was not associated with GnRH agonist overuse (odds ratio (OR) 0.89; 95% confidence interval (CI): 0.75–1.05). However, solo practice type (OR 1.65; 95% CI: 1.34–2.02), medical school affiliation (OR 0.65; 95% CI: 0.55–0.77) and patient race were. Compared with non-Hispanic whites, non-Hispanic blacks (OR 1.76; 95% CI: 1.37–2.27), Hispanics (OR 1.41; 95% CI: 1.12–1.79) and men of ‘other’ race (OR 1.44; 95% CI: 1.04–1.99) had greater odds of receiving unnecessary GnRH agonists.
Conclusions:
GnRH agonist overuse remains high among some urologists who may be professionally isolated and difficult to reach. These urologists treat more vulnerable populations, which may contribute to health disparities in prostate cancer treatment quality. Nonetheless, these findings provide guidance to develop interventions to address overuse in prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wilt TJ, Shamliyan T, Taylor B, MacDonald R, Tacklind J, Rutks I, et al Comparative Effectiveness of Therapies for Clinically Localized Prostate Cancer. Agency for Healthcare Research and Quality. Rockville, MD, 2008; Report No.: 08-EHC010-EF; Contract No.: 08-EHC010-EF.
National Cancer Institute. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute: Bethesda, MD, 2010.
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML . Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 2011; 103: 117–128.
Bahnson RR, Hanks GE, Huben RP, Kantoff P, Kozlowski JM, Kuettel M, et al. NCCN Practice Guidelines for prostate cancer. Oncology (Williston Park) 2000; 14: 111–119.
Pagliarulo V, Bracarda S, Eisenberger MA, Mottet N, Schroder FH, Sternberg CN, et al. Contemporary role of androgen deprivation therapy for prostate cancer. Eur Urol 2012; 61: 11–25.
Leape LL, Berwick DM . Five years after To Err Is Human: what have we learned? JAMA 2005; 293: 2384–2390.
National Comprehensive Cancer Network. Prostate Cancer, National Comprehensive Cancer Network, Fort Washington, PA, 2004.
Elliott SP, Jarosek SL, Wilt TJ, Virnig BA . Reduction in physician reimbursement and use of hormone therapy in prostate cancer. J Natl Cancer Inst 2010; 102: 1826–1834.
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS . Determinants of androgen deprivation therapy use for prostate cancer: role of the urologist. J Natl Cancer Inst 2006; 98: 839–845.
Keating NL . Medicare reimbursement and prescribing hormone therapy for prostate cancer. J Natl Cancer Inst 2010; 102: 1814–1815.
Jacobson M, O'Malley AJ, Earle CC, Pakes J, Gaccione P, Newhouse JP . Does reimbursement influence chemotherapy treatment for cancer patients? Health Aff (Millwood) 2006; 25: 437–443.
Jacobson M, Earle CC, Price M, Newhouse JP . How Medicare's payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Aff (Millwood) 2010; 29: 1391–1399.
Shahinian VB, Kuo YF, Gilbert SM . Reimbursement policy and androgen-deprivation therapy for prostate cancer. N Engl J Med 2010; 363: 1822–1832.
O'Leary MP, Baum NH, Bohnert WW, Blizzard R, Bonney WW, Cooper TP, et al. 2003 American Urological Association Gallup survey: physician practice patterns, cryosurgery/brachytherapy, male infertility, female urology and insurance/professional liability. J Urol 2004; 171: 2363–2365.
Choudhry NK, Fletcher RH, Soumerai SB . Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med 2005; 142: 260–273.
Quessential Medical Market Research. Physician Outlook: Urology. Exeter, NH: Quessential Medical Market Research, 2013.
Damiani G, Silvestrini G, Federico B, Cosentino M, Marvulli M, Tirabassi F, et al. A systematic review on the effectiveness of group versus single-handed practice. Health Policy 2013; 113: 180–187.
National Cancer Institute SEER-Medicare. National Cancer Institute: Bethesda, MD, 2011.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF . Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 2002; 40, IV-3–18.
Office of Information Products and Data Analysis (OIPDA) Medicare and medicaid statistical supplement, 2013. In: Services CfMaM (ed). Centers for Medicare and Medicaid Services: Baltimore, MD, 2013.
Baldwin LM, Adamache W, Klabunde CN, Kenward K, Dahlman C, J LW . Linking physician characteristics and medicare claims data: issues in data availability, quality, and measurement. Med Care 2002; 40, IV- 82–95.
Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol 2007; 177: 2106–2131.
National Comprehensive Cancer Network. Prostate Cancer, National Comprehensive Cancer Network, Fort Washington, PA, 2008.
Freiman MP . The rate of adoption of new procedures among physicians. The impact of specialty and practice characteristics. Med Care 1985; 23: 939–945.
Wright JD, Neugut AI, Wilde ET, Buono DL, Malin J, Tsai WY, et al. Physician characteristics and variability of erythropoiesis-stimulating agent use among Medicare patients with cancer. J Clin Oncol 2011; 29: 3408–3418.
Reid RO, Friedberg MW, Adams JL, McGlynn EA, Mehrotra A . Associations between physician characteristics and quality of care. Arch Intern Med 2010; 170: 1442–1449.
Shahinian VB, Kuo YF, Freeman JL, Orihuela E, Goodwin JS . Characteristics of urologists predict the use of androgen deprivation therapy for prostate cancer. J Clin Oncol 2007; 25: 5359–5365.
Pollack CE, Bekelman JE, Liao KJ, Armstrong K . Hospital racial composition and the treatment of localized prostate cancer. Cancer 2011; 117: 5569–5578.
Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D . A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol 2007; 17: 584–590.
Klabunde CN, Potosky AL, Legler JM, Warren JL . Development of a comorbidity index using physician claims data. J Clin Epidemiol 2000; 53: 1258–1267.
Elliott SP, Johnson DP, Jarosek SL, Konety BR, Adejoro OO, Virnig BA . Bias due to missing SEER data in D'Amico risk stratification of prostate cancer. J Urol 2012; 187: 2026–2031.
Feldstein PJ . Health Policy Issues: An Economic Perspective, 4th edn. Health Administration Press: Chicago, IL, 2007.
Jang TL, Bekelman JE, Liu Y, Bach PB, Basch EM, Elkin EB, et al. Physician visits prior to treatment for clinically localized prostate cancer. Arch Intern Med 2010; 170: 440–450.
Raudenbush S, Bryk A . Hierarchical Linear and Nonlinear Modeling. Sage Publications: Thousand Oaks, CA, 2002.
StataCorp LP . Stata/IC 12.1 for Windows. StataCorp LP: College Station, TX, 2013.
D'Amico AV, Whittington R, Malkowicz SB, Wu YH, Chen M, Art M, et al. Combination of the preoperative PSA level, biopsy gleason score, percentage of positive biopsies, and MRI T-stage to predict early PSA failure in men with clinically localized prostate cancer. Urology 2000; 55: 572–577.
Arias E . United States life tables, 2000. Natl Vital Stat Rep 2002; 51: 1–38.
Arias E . United States life tables, 2002. Natl Vital Stat Rep 2004; 53: 1–38.
Arias E . United States life tables, 2001. Natl Vital Stat Rep 2004; 52: 1–38.
Arias E . United States life tables, 2003. Natl Vital Stat Rep 2006; 54: 1–40.
Arias E . United States life tables, 2004. Natl Vital Stat Rep 2007; 56: 1–39.
Arias E . United States life tables, 2006. Natl Vital Stat Rep 2010; 58: 1–40.
Arias E . United States life tables, 2007. Natl Vital Stat Rep 2011; 59: 1–60.
Ganz PA, Barry JM, Burke W, Col NF, Corso PS, Dodson E, et al. National Institutes of Health State-of-the-Science Conference: role of active surveillance in the management of men with localized prostate cancer. Ann Intern Med 2012; 156: 591–595.
Eccles MP, Foy R, Sales A, Wensing M, Mittman B . Implementation Science six years on—our evolving scope and common reasons for rejection without review. Implement Sci 2012; 7: 71.
Mehrotra A, Reid RO, Adams JL, Friedberg MW, McGlynn EA, Hussey PS . Physicians with the least experience have higher cost profiles than do physicians with the most experience. Health Aff (Millwood) 2012; 31: 2453–2463.
Scott SD, Plotnikoff RC, Karunamuni N, Bize R, Rodgers W . Factors influencing the adoption of an innovation: an examination of the uptake of the Canadian Heart Health Kit (HHK). Implement Sci 2008; 3: 41.
Vaughan A, Coustasse A . Accountable care organization musical chairs: will there be a seat remaining for the small group or solo practice? [corrected]. Hosp Top 2011; 89: 92–97.
Borges NJ, Navarro AM, Grover A, Hoban JD . How, when, and why do physicians choose careers in academic medicine? A literature review. Acad Med 2010; 85: 680–686.
Neuwahl S, Thompson K, Fraher E, Ricketts T . HPRI data tracks. Urology workforce trends. Bull Am Coll Surg 2012; 97: 46–49.
Nathan H, Pawlik TM, Wolfgang CL, Choti MA, Cameron JL, Schulick RD . Trends in survival after surgery for cholangiocarcinoma: a 30-year population-based SEER database analysis. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2007; 11: 1488–1496; discussion 96–97.
Virnig B (ed). SEER-Medicare Training Workshop. SEER-Medicare Training Workshop. National Institutes of Health: Bethesda, MD, 2011.
Virnig BA, Warren JL, Cooper GS, Klabunde CN, Schussler N, Freeman J . Studying radiation therapy using SEER-Medicare-linked data. Med Care 2002; 40, IV 49–54.
Cooper GS, Virnig B, Klabunde CN, Schussler N, Freeman J, Warren JL . Use of SEER-Medicare data for measuring cancer surgery. Med Care 2002; 40, IV 43–48.
Lund JL, Sturmer T, Harlan LC, Sanoff HK, Sandler RS, Brookhart MA, et al. Identifying specific chemotherapeutic agents in Medicare data: a validation study. Med Care 2013; 51: e27–e34.
Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S . Overuse of health care services in the United States: an understudied problem. Arch Intern Med 2012; 172: 171–178.
National Priorities Partnership National Priorities and Goals: Aligning Our Efforts to Transform America’s Healthcare. Washington, DC, 2008.
National Priorities Partnership Input to the Secretary of Health and Human Services on Priorities for the National Quality Strategy. National Quality Forum: Washington, DC, 2011.
Acknowledgements
This study was peer-reviewed and presented at the American Society of Clinical Oncology in June 2014. Work on this study was supported by the Integrated Cancer Information and Surveillance System (ICISS), UNC Lineberger Comprehensive Cancer Center with funding provided by the University Cancer Research Fund (UCRF) via the State of North Carolina. The American Medical Association is the source for the raw physician data. The National Cancer Institute provided the SEER-Medicare linked data and reviewed the manuscript for potential privacy violations. The collection of the California cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Souther0n California and contract N02-PC-15105 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement no. U55/CCR921930-02 awarded to the Public Health Institute. The statistics, tables, ideas and opinions expressed herein are those of the author(s) and endorsement by the American Medical Association, State of California, Department of Public Health the National Cancer Institute and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred. We acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS) Inc.; and the Surveillance, Epidemiology and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. Dr Ellis was supported by a National Cancer Institute training grant (R25CA116339) and a University of North Carolina Lineberger Comprehensive Cancer Center Dissertation Completion Award. Dr Nielsen was supported in part by The American Cancer Society (grant number MRSG-13-154-01-CPPB) and The Urology Care Foundation/Astellas (Rising Stars in Urology Research Award). Dr Weinberger was supported by a Senior Research Career Scientist Award (91–408) from the US Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
About this article
Cite this article
Ellis, S., Nielsen, M., Carpenter, W. et al. Gonadotropin-releasing hormone agonist overuse: urologists’ response to reimbursement and characteristics associated with persistent overuse. Prostate Cancer Prostatic Dis 18, 173–181 (2015). https://doi.org/10.1038/pcan.2015.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.10
This article is cited by
-
Perceived barriers to the adoption of active surveillance in low-risk prostate cancer: a qualitative analysis of community and academic urologists
BMC Cancer (2021)
-
Determinants for the use and de-implementation of low-value care in health care: a scoping review
Implementation Science Communications (2021)