Abstract
Background
Increasing national expenditures and use associated with TKA have resulted in pressure to reduce costs through various reimbursement cuts. However, within the arthroplasty literature, few studies have examined the association of medical comorbidities on resource use and length of stay after joint arthroplasty.
Questions/purposes
The purpose of this study was to examine the association between individual patient characteristics (including demographic factors and medical comorbidities) on resource allocation and length of stay (LOS) after TKA.
Methods
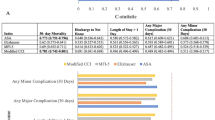
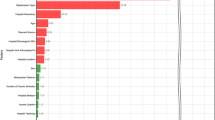
We queried the 2009 Nationwide Inpatient Sample dataset for International Classification of Diseases, 9th Revision code, 81.54, for TKAs. An initial 621,029-patient cohort was narrowed to 516,745 after inclusion of elective TKAs on patients aged between 40 and 95 years. Using generalized linear models, we estimated the effect of comorbidities on resource use (using cost-to-charge conversions to estimate hospital costs) and the LOS controlling for patient and hospital characteristics. Across the 2009 national cohort with TKAs, 12.7% had no comorbidities, whereas 32.6% had three or more. The most common conditions included hypertension (67.8%), diabetes (20.0%), and obesity (19.8%). Mean hospital costs were USD 14,491 (95% confidence interval [CI], 14,455–14,525) and mean hospital LOS was 3.3 days (95% CI, 3.29–3.31) in this data set.
Results
Patients with multiple comorbidities were associated with increased resource use and LOS. Higher marginal costs and LOS were associated with patients who had an inpatient death (USD +8017 [95% CI, 8006–8028], +2.3 [CI, 2.15–2.44] days over baseline), patients with recent weight loss (USD +4587 [95% CI, 4581–4593], +1.5 [CI, 1.45–1.61) days], minority race (USD +1037 [95% CI, 1035–1038], +0.3 [CI, 0.28–0.33] days), pulmonary-circulatory disorders (USD +3218 [95% CI, 3214–3221], +1.3 [CI, 1.25–1.34] days), and electrolyte disturbances (USD +1313 [95% CI, 1312–1314], +0.6 [CI, 0.57–0.60] days). All p values were < 0.001.
Conclusion
Multiple patient comorbidities were associated with additive resource use and LOS after TKA. Current reimbursement may not adequately account for these patient characteristics. To avoid potential loss of access to care for sicker patients, payment needs to be adjusted to reflect actual resource use.
Level of Evidence
Level IV, economic and decision analysis. See the Instructions for Authors for a complete description of levels of evidence.




Similar content being viewed by others
References
Atkinson JG. Flaws in the Medicare readmission penalty. N Engl J Med. 2012;367:2056–2057.
Baser O, Fan Z, Dimick JB, Staiger DO, Birkmeyer JD. Outlier payments for cardiac surgery and hospital quality. Health Aff (Millwood). 2009;28:1154–1160.
Bozic KJ, Lau E, Kurtz S, Ong K, Rubash H, Vail TP, Berry DJ. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Joint Surg Am. 2012;94:794–800.
Bozic KJ, Rubash HE, Sculco TP, Berry DJ. An analysis of medicare payment policy for total joint arthroplasty. J Arthroplasty. 2008;23:133–138.
Cai X, Cram P, Vaughan-Sarrazin M. Are African American patients more likely to receive a total knee arthroplasty in a low-quality hospital? Clin Orthop Relat Res. 2012;470:1185–1193.
Chen LT, Lee JA, Chua BS, Howe TS. Hip fractures in the elderly: the impact of comorbid illnesses on hospitalisation costs. Ann Acad Med Singapore. 2007;36:784–787.
CMS. CMS dry run hospital-specific report for hospital-wide all-cause unplanned readmission (HWR) Measure. 2012. Available at: www.cms.gov. Accessed October 1, 2013.
CMS. Acute Care hospital inpatient prospective payment system. Centers For Medicare and Medicaid Services. 2013. Available at: http://www.cms.gov/Medicare/Medicare-Fee-For-Service-Payment/AcuteInpatientPPS. Accessed October 1, 2013.
Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–259.
Cram P, Ibrahim SA, Lu X, Wolf BR. Impact of alternative coding schemes on incidence rates of key complications after total hip arthroplasty: a risk-adjusted analysis of a national data set. GeriatriOrthop Surg Rehabil. 2012;3:17–26.
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Gruskay JA, Fu MC, Bohl DD, Webb ML, Grauer JN. Factors affecting length of stay following elective posterior lumbar spine surgery: a multivariate analysis. Spine J. 2013 Nov 1. pii: S1529-9430(13)01617-3. doi: 10.1016/j.spinee.2013.10.022 [Epub ahead of print].
HCUP. Overview of the National Inpatient Sample (NIS). Agency for Healthcare Research and Quality. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed April 14, 2013.
Ho DM, Huo MH. Are critical pathways and implant standardization programs effective in reducing costs in total knee replacement operations? J Am Coll Surg. 2007;205:97–100.
Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J. The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty. 2013;28:21–24.
Joynt KE, Jha AK. Thirty-day readmissions—truth and consequences. N Engl J Med. 2012;366:1366–1369.
Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–681.
Kelly MP, Bozic KJ. Cost drivers in total hip arthroplasty: effects of procedure volume and implant selling price. Am J Orthop (Belle Mead NJ). 2009;38:E1–4.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Li Y, Lu X, Wolf BR, Callaghan JJ, Cram P. Variation of Medicare Payments for Total Knee Arthroplasty. J Arthroplasty. 2013;28:1513–1520.
Lin CA, Takemoto S, Kandemir U, Kuo AC. Mid-term outcomes in HIV-positive patients after primary total hip or knee arthroplasty. J Arthroplasty. 2014;29:277–282.
Maradit Kremers H, Visscher SL, Kremers WK, Naessens JM, Lewallen DG. Obesity increases length of stay and direct medical costs in total hip arthroplasty. Clin Orthop Relat Res. 2014;472:1232–1239.
Monsef JB, Della Valle AG, Mayman DJ, Marx RG, Ranawat AS, Boettner F. The impact of blood management on length of stay after primary total knee arthroplasty. Open Orthop J. 2014;8:108–113.
Nikkel LE, Fox EJ, Black KP, Davis C, Andersen L, Hollenbeak CS. Impact of comorbidities on hospitalization costs following hip fracture. J Bone Joint Surg Am. 2012;94:9–17.
Norian JM, Ries MD, Karp S, Hambleton J. Total knee arthroplasty in hemophilic arthropathy. J Bone Joint Surg Am. 2002;84:1138–1141.
Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95:193–199.
Robinson JC, Pozen A, Tseng S, Bozic KJ. Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am. 2012;94:1693–1698.
Shah AN, Vail TP, Taylor D, Pietrobon R. Comorbid illness affects hospital costs related to hip arthroplasty: quantification of health status and implications for fair reimbursement and surgeon comparisons. J Arthroplasty. 2004;19:700–705.
Shwartz M, Iezzoni LI, Moskowitz MA, Ash AS, Sawitz E. The importance of comorbidities in explaining differences in patient costs. Med Care. 1996;34:767–782.
Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2013 18 Sep [Epub ahead of print].
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
The study examined inpatient admissions in 2009 using the National Inpatient Sample (NIS) Database, Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. The HCUP and the hospitals participating in the NIS Program are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Pugely, A.J., Martin, C.T., Gao, Y. et al. Comorbidities in Patients Undergoing Total Knee Arthroplasty: Do They Influence Hospital Costs and Length of Stay?. Clin Orthop Relat Res 472, 3943–3950 (2014). https://doi.org/10.1007/s11999-014-3918-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3918-x