Abstract
Background
Bedside rounds have decreased in frequency on teaching services. Perceived barriers toward bedside rounds are inefficiency and patient and house staff lack of preference for this mode of rounding.
Objectives
To evaluate the impact of a bedside rounding intervention on the frequency of bedside rounding, duration of patient encounters and rounding sessions, and patient and resident attitudes toward bedside rounds.
Design
A pre- and postintervention design, with a bedside rounding workshop midway through two consecutive internal medicine rotations, with daily resident interviews, patient surveys, and an end-of-the-year survey given to all Medicine house staff.
Participants
Medicine house staff and medicine patients.
Measures
Frequency of bedside rounds, duration of new patient encounters and rounding sessions, and patient and house staff attitudes regarding bedside rounds.
Results
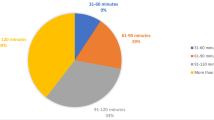
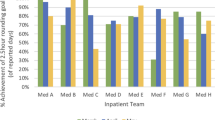
Forty-four residents completed the bedside rounding workshop. Comparing the preintervention and postintervention phases, bedside rounds increased from <1% to 41% (p < 0.001). The average duration of walk rounding encounters was 16 min, and average duration of bedside rounding encounters was 15 min (p = 0.42). Duration of rounds was 95 and 98 min, respectively (p = 0.52). Patients receiving bedside rounds preferred bedside rounds (99% vs. 83%, p = 0.03) and perceived more time spent at the bedside by their team (p < 0.001). One hundred twelve house staff (71%) responded, with 73% reporting that bedside rounds are better for patient care. House staff performing bedside rounds were less likely to believe that bedside rounds were more educational (53% vs. 78%, p = 0.01).
Conclusions
Bedside rounding increased after an educational intervention, and the time to complete bedside rounding encounters was similar to alternative forms of rounding. Patients preferred bedside rounds and perceived more time spent at the bedside when receiving bedside rounds. Medicine residents performing bedside rounds were less likely to believe bedside rounds were more educational, but all house staff valued the importance of bedside rounding for the delivery of patient care.

Similar content being viewed by others
References
Osler W. On the need of radical reform in our methods of teaching senior residents. Medical News. 1903;(82):49-53.
Linfors EW, Neelon FA, Sounding Boards. The case of bedside rounds. N Engl J Med. 1980;303(21):1230–1233.
Thayer W. Osler the Teacher. Bull Johns Hopkins Hospital. 1919.;30(303):198-200 (1980; 1303:1230-1983).
Collins GF, Cassie JM, Daggett CJ. The role of the attending physician in clinical training. J Med Educ. 1978;53(5):429–431.
Gonzalo JD, Masters PA, Simons RJ, Chuang CH. Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110.
Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748–2751.
Ramani S. Twelve tips to improve bedside teaching. Med Teach. 2003;25(2):112–115.
Alpert JS. Some thoughts on bedside teaching. Am J Med. 2009;122(3):203–204.
Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside teaching? A focus-group study of clinical teachers. Acad Med. 2003;78(4):384–390.
Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257–264.
Nair BR, Coughlan JL, Hensley MJ. Impediments to bed-side teaching. Med Educ. 1998;32(2):159–162.
Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4(5):304–307.
Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945–949.
Romano J. Patient's attitude and behavior in ward round teaching. J Am Med Assoc. 1941;(117):664-667.
Wang-Cheng RM, Barnas GP, Sigmann P, Riendl PA, Young MJ. Bedside case presentations: why patients like them but learners don’t. J Gen Intern Med. 1989;4(4):284–287.
Lehmann LS, Brancati FL, Chen MC, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155.
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet. 2002;360(9350):2026–2030.
Birnbaumer D, MD, FACEP. Bedside Teaching, The Teaching Microskills, and the Teachable Moment. [Online powerpoint presentation.]; 2007. www.acep.org.
Aldeen AZ, Gisondi MA. Bedside teaching in the emergency department. Acad Emerg Med. 2006;13(8):860–866.
Weinholtz D, Edwards JC, Mumford LM. Teaching during rounds: a handbook for attending physicians and residents. Baltimore: Johns Hopkins University Press; 1992.
Acknowledgements
The authors would like to thank Dr. Shoshana Herzig for assistance with survey design and implementation. Also, the authors would like to thank the Internal Medicine residents of the Beth Israel Deaconess Medical Center for their dedication to patient care and their willingness to contribute to this study. The project was presented, in part, as an oral presentation at the SGIM Annual Meeting, Miami, FL, May 15, 2009.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix I
”Tips for Bedside Rounding” Handout18–20
Before Rounding Session:
-
Prepare for patient cases before rounds
-
Decide with team which patients are appropriate for bedside rounds
-
Orient learners—ensure everyone knows what is expected of them
-
Prepare patients prior to rounds, when possible
-
Invite patient’s nurse if feasible
During Rounding Session:
-
Have patient’s doctor (resident, student, etc.) introduce all members of the team
-
Orient patient and learners—encourage patient to correct/contribute to details
-
Position patient appropriately; position team around bedside
-
Do not avoid sensitive material
-
Allow interruptions by patient and learners
-
Examine pertinent or illustrative parts−invite students to participate
-
Discuss events, labs, assessment, plan
-
Challenge intellectually with open-ended questions
-
Use “teachable moments” when available
-
Teach to all levels of learners and encourage all to participate
-
“I don’t know” is an appropriate answer
-
Communicate and summarize plan for patient and team
After Rounding Session:
-
Debrief sessions when appropriate
-
Offer time to clarify questions or address remaining issues after session
-
Offer feedback to reinforce positive skills demonstrated at bedside
Appendix II
Patient Survey Items.
-
1.
Introductory statements:
-
For patients not receiving bedside rounds: “Your Medicine team of doctors discussed your case outside of your room, then updated you about the plan.”
-
For patients receiving bedside rounds: “Your Medicine team of doctors discussed your case at the bedside in your presence.”
-
2.
What is your ethnic background (circle one):
-
Black/African-American
-
White
-
Asian
-
Other
-
3.
Which language do you consider your primary language?
-
English
-
Spanish
-
Russian
-
Other
-
4.
“In reference to the degree of respect your medicine team showed during your stay, please choose:”
-
a.
Significant Gain of Respect—respect almost always demonstrated
-
b.
Moderate Gain of Respect—most of the time, I was treated with respect
-
c.
Mild Gain of Respect—I often experienced a sense of respect
-
d.
No sense of loss or gain of respect
-
e.
Mild Loss of Respect—I often experienced low-grade loss of respect
-
f.
Moderate Loss of Respect—almost most of the time, I had concerns about disrespectful behavior
-
g.
Significant Loss of Respect—sense of loss of respect was almost always present
-
5.
Please comment on the statement: “Your Medicine team used confusing terms.”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
6.
Please comment on the statement: “I would prefer my medicine team of doctors to round as a team at the bedside during morning rounds”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
7.
Please comment on the statement: “My medicine team involved me with medical decisions.”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
8.
How many minutes per morning were at least two of your physicians together at the bedside with you?
-
zero minutes
-
1 to 5 minutes
-
6 to 10 minutes
-
11 to 15 minutes
-
16 to 20 minutes
-
21-25 minutes
-
25+ minutes
Rights and permissions
About this article
Cite this article
Gonzalo, J.D., Chuang, C.H., Huang, G. et al. The Return of Bedside Rounds: An Educational Intervention. J GEN INTERN MED 25, 792–798 (2010). https://doi.org/10.1007/s11606-010-1344-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1344-7