Abstract
Objective
Whether chest radiographs (CXRs) in mechanically ventilated patients should be routinely obtained or only when an abnormality is anticipated remains debated. We aimed to compare the diagnostic, therapeutic and outcome efficacy of a restrictive prescription of CXRs with that of a routine prescription, focusing on delayed diagnoses and treatments potentially related to the restrictive prescription.
Design
Randomized controlled trial.
Setting
Intensive care unit of the Avicenne Teaching Hospital, Bobigny, France.
Patients and participants
All consecutive patients mechanically ventilated for ≥ 48 h between January and June 2006.
Interventions
Patients were randomly assigned to have daily routine CXRs (routine prescription group) or clinically indicated CXRs (restrictive prescription group).
Measurements and results
For each CXR, a questionnaire was completed addressing the reason for the CXR, the new findings, and any subsequent therapeutic intervention. The endpoints were the rates of new findings, the rates of new findings that prompted therapeutic intervention, the rate of delayed diagnoses, and mortality. Eighty-four patients were included in the routine prescription group and 81 in the restrictive prescription group. The rates of new findings and the rates of new findings that prompted therapeutic intervention in the restrictive prescription group and in the routine prescription group were 66% vs. 7.2% (p < 0.0001), and 56.4% vs. 5.5% (p < 0.0001) respectively. The rate of delayed diagnoses in the restrictive prescription group was 0.7%. Mortality was similar.
Conclusions
Restrictive use of CXRs in mechanically ventilated patients was associated with better diagnostic and therapeutic efficacies without impairing outcome.
Similar content being viewed by others
Introduction
Invasive mechanical ventilation (MV) is a frequent issue in critically ill patients. Chest radiographs (CXRs) are routinely performed in these patients to verify the right position of the endotracheal tube (ETT) or central venous devices, and to diagnose complications such as ventilator-associated pneumonia (VAP), pulmonary edema, and pneumothorax. Yet, whether CXRs should be obtained on a daily basis or only when there is a clinical suspicion that an abnormality will be present remains debated. There are two different schools of thought regarding this topic. Some have advocated ordering daily routine CXRs by claiming that the incidence of unsuspected abnormalities is high [1–3]. Others have suggested that protocols mandating daily routine CXRs are not cost-effective and can be safely abandoned [4–8]. As a consequence, standards of care vary from one institution to another and, sometimes, even within a given institution.
Available studies on daily routine CXRs do not allow an accurate estimation of the benefit--risk ratio. Daily routine CXRs seem to rarely reveal major findings likely to prompt therapeutic intervention [9]. Besides, they carry the risk that minor findings or false-positive findings might be acted upon [10]. Thus, a rational use of CXRs based on clinical evaluation may be preferable.
To our knowledge, a single study in adult patients has compared the outcome efficacy of daily routine CXRs (routine prescription) with that of clinically indicated CXRs (restrictive prescription). The proportion of new findings that prompted therapeutic intervention was lower in the routine prescription group, whereas patients' outcomes were similar [11].
However, it was not clear whether the diagnosis of serious events such as VAP, pulmonary edema or pneumothorax might have been delayed in the restrictive prescription group (i. e., if a serious event had occurred between two clinically indicated CXRs). Since delayed diagnosis and treatment of such events may be associated with a worse outcome, we thought it important to further evaluate this issue. Therefore, we carried out a study to assess not only the efficacy, but also the safety of a restrictive prescription of CXRs.
Materials and methods
Study design and setting
This prospective, randomized, controlled study was performed in the medical and surgical intensive care unit (ICU) of the Avicenne Teaching Hospital (Bobigny, France).
The study design was approved by the local ethics committee and conformed to ethical guidelines (Declaration of Helsinki) and the International Conference on Harmonization (ICH).
Patients
All consecutive patients admitted to our ICU between January and June 2006 who received invasive MV were eligible. They were included in the study if their duration of MV was 48 h or more. Patients with a shorter duration of MV were not included, since CXRs are commonly obtained for various reasons within the first 48 h of intubation. Patients who required reintubation (except after unplanned extubation), patients who were ventilated through a tracheostomy tube (who represent a particular subset of mechanically ventilated patients), and patients in whom a decision to withhold or withdraw life-sustaining treatments was made were also excluded to minimize the risk of confounding.
Patients were followed up until discharge from hospital or death. Once discharged from the ICU, they were considered to be unqualified for reenrollment in the study in the event that they required a new admission.
Procedures and data collection
After 48 h of MV, patients were randomly allocated to have daily routine CXRs (routine prescription group) or clinically indicated CXRs (restrictive prescription group). Randomization was performed using a computer-generated random number table. Figure 1 summarizes the sequence of eligibility and randomization.
All CXRs were obtained with conventional film-based portable equipment and were of an antero-posterior view.
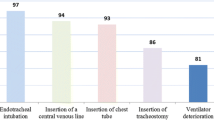
For each CXR performed, a specially developed checklist was used to document the reason for the CXR (none, suspected VAP, change in auscultation, increased plateau pressures, or change in blood gas values), the new findings (VAP, pulmonary edema, atelectasis, pneumothorax,pleural effusion, misplacement of the ETT, or any other finding), and the subsequent therapeutic intervention (antibiotic therapy, adjunction of diuretics or dobutamine, bronchoscopy procedure, thoracentesis, or any other therapeutic intervention).
The attending physicians met daily, as soon as CXRs were available, to assess the new findings (the attending physicians and not a radiologist interpreted the CXRs to avoid any interference with our current practice and better reflect “real life”) and decide whether any therapeutic intervention was required.
Other data collected were: age, gender, McCabe class (class 1, no fatal underlying disease; class 2, underlying disease fatal within 5 years; class 3, underlying diseasefatal within 1 year), SAPS II score, APACHE II score, admission category (medical, scheduled surgery, or unscheduled surgery), comorbidities, reason for initiation of MV, number of ventilation-free days, lengths of ICU and hospital stays, and vital status at ICU and hospital discharge.
In both groups, CXRs were usually obtained between 9 and 11 a.m. Additional CXRs could be obtained on a 24-h basis, if deemed necessary by the attending physician.
In the routine prescription group, CXRs were ordered and interpreted daily, irrespective of whether an abnormality was anticipated. In the restrictive prescription group, CXRs were also obtained on a daily basis. They were interpreted only if an abnormality was anticipated (clinically indicated CXRs). The remaining CXRs (non-clinically indicated CXRs) were kept hidden from the investigators and interpreted retrospectively after completion of the study to assess whether any serious pleuropulmonary event had occurred between two clinically indicated CXRs. For safety considerations, non-clinically indicated CXRs could be read immediately in the case of acute worsening of the patients' cardiopulmonary state.
Chest radiographs performed after the insertion of central venous devices or nasogastric tubes (NGT) were not taken into account in the final analysis. They were interpreted by junior physicians not involved in the study to avoid any bias.
The endpoints that we evaluated were: the rates of new findings (number of CXRs with new findings/number of routine or clinically indicated CXRs), the rates of new findings that prompted therapeutic intervention (number of CXRs with new findings that prompted therapeutic intervention/number of routine or clinically indicated CXRs), the rate of delayed diagnoses in the restrictive prescription group (number of retrospective diagnoses/number of non-clinically indicated CXRs), and ICU and hospital mortality.
Since no consensus exists on the timing of and indications for CXRs in mechanically ventilated patients in the current medical literature, the present study did not involve any change in patient management. Moreover, CXRs were always available for every patient. The patients, or their next of kin, were given information about the protocol, but signed informed consent was waived.
Statistical analysis
When using a restrictive prescription, the rate of new findings on CXRs is likely to reach 50% [11]. In contrast, the rate of new findings on routine CXRs has been reported to be as low as 6% [9]. The true difference being probably somewhere in between, we calculated that 80 patients per group would need to be enrolled to have a statistical power of 90% to detect an absolute difference of 25% in the rate of new findings between the restrictive prescription and the routine prescription groups.
Results are expressed as means and standard deviations for continuous variables and as numerical values and percentages for categorical variables. Comparisons between groups were based on the Student's t test for continuous variables and on the Chi-squared or Fisher's exact test for categorical variables.
All p values were two-tailed, and p < 0.05 was considered significant. Statistical analyses were performed using a statistical software package (SAS, version 9.1; SAS Institute, Cary, NC, USA).
Results
Patients
One hundred and ninety-one patients were eligible. Twenty-six patients were excluded for the following reasons: mechanical ventilation for less than 48 h (n = 12), the need for reintubation (n = 8), the decision to withhold or withdraw life-sustaining treatments (n = 5), and ventilation through a tracheostomy tube (n = 1). Finally, 165 patients were included, of whom 84 were allocated to the routine prescription group and 81 to the restrictive prescription group (Fig. 1). Baseline characteristics were similar in both groups. In particular, there was no difference with regard to age, gender, severity scores, and reason for initiation of mechanical ventilation (Table 1).
Diagnostic efficacy
In the restrictive prescription group, 94 clinically indicated CXRs were obtained, 62 of which revealed a new finding. The retrospective analysis of non-clinically indicated CXRs showed that a diagnosis could have been made 24 h earlier in 6 patients if a systematic CXR had been obtained, yielding a 0.7% rate of delayed diagnoses (6 out of 849). These 6 patients had minor atelectases, which did not prompt any therapeutic intervention. In 25 cases, a non-clinically indicated CXR was read before termination of the study because of a sudden decrease in arterial O2 saturation measured by pulse oximetry, but did not reveal any new findings.
In the routine prescription group, most CXRs were not helpful. Of the 885 CXRs obtained, only 64 revealed new findings.
Accordingly, the rates of new findings in the restrictive prescription group and in the routine prescription group were 66% and 7.2% respectively. The difference between the two groups was highly significant (p < 0.0001). However, if only clinically indicated CXRs from the routine prescription group were analyzed, the rate of new findings rose up to 69.6% (64 out of 92) and there was no further difference between the two groups (66% vs. 69.6%, p = 0.6).
Details of the new findings in the two groups are shown in Table 2.
Therapeutic efficacy
Of the 94 clinically indicated CXRs obtained in the restrictive prescription group, 53 revealed new findings important enough to prompt therapeutic intervention.
Of the 885 CXRs obtained in the routine prescription group, only 49 revealed a new finding important enough to prompt therapeutic intervention.
Accordingly, the rates of new findings that prompted therapeutic intervention in the restrictive prescription group and in the routine prescription group were 56.4% and 5.5% respectively. The difference between the two groups was highly significant (p < 0.0001). However, if only clinically indicated CXRs from the routine prescription group were analyzed, the rate of new findings that prompted therapeutic intervention rose to 53.3% (49 out of 92) and there was no further difference between the two groups (56.4% vs. 53.3%, p = 0.7).
Details of therapeutic intervention in the two groups are shown in Table 2.
Outcome efficacy
The gain in diagnostic and therapeutic efficacy observed in the restrictive prescription group did not worsen patients' outcomes. Actually, there were no differences between the two groups in terms of ICU mortality, hospital mortality, number of ventilation-free days, duration of ICU stay, and duration of hospital stay (Table 3).
Discussion
Our study shows that restrictive use of CXRs is effective and safe. The diagnostic and therapeutic efficacies were much higher in the restrictive prescription group than in the routine prescription group, and the outcome was similar between the two groups. As a consequence, protocols advocating routine CXRs in mechanically ventilatedpatients could be safely abandoned, and CXRs should instead be performed when a significant abnormality is anticipated. The fact that differences in diagnostic and therapeutic efficacies were abolished if only clinically indicated CXRs from the routine prescription group were analyzed strengthens our conclusions.
Despite CXR being a very common procedure in the ICU, only few studies have evaluated its actual value. Most of these studies were observational cohort studies assessing the incidence and nature of the new diagnoses made on daily routine CXRs [2, 3, 5, 6, 8, 9]. Overall, the new findings mainly consisted of ETT or NGT malpositioning and rarely resulted in significant therapeutic interventions. It must be emphasized that none of these studies compared daily routine CXRs with non-routine CXRs with regard to diagnostic, therapeutic or outcome efficacy, thus precluding drawing any definite conclusion.
To our knowledge, a single study has compared routine with non-routine CXRs in adult ICU patients [11]. The results were similar to ours. However, no details about potentially delayed diagnoses and treatments related to the restrictive prescription were provided.
The main strength of our study was to focus on the problem of potentially delayed diagnoses and treatment of serious events that could have worsened patients' outcome in the restrictive prescription group. Actually, the higher diagnostic and therapeutic efficacy of the restrictive strategy was expected. But the concern that those who continue to perform daily CXRs have is about safety. They worry about the potential to miss an important diagnosis by not having a daily CXR. Our findings were reassuring in that only six minor atelectases (that did not require a bronchoscopy procedure) were diagnosed with a 24-h delay in the restrictive prescription group without any negative impact. In addition, there was no difference between the two groups regarding relevant outcome endpoints (mortality, length of stay, and ventilation-free days). Another strength was that the two groups in our study were well balanced with respect to baseline characteristics, underlying diseases, and reason for MV. In contrast, there were some differences between groups in the study by Krivopal et al. [11]. As the authors stated, these differences, although not statistically significant, may have brought about some confusion. Finally, we included both medical and surgical patients, thus reinforcing the external validity of our results.
In keeping with previous reports, the rate of new findings in the routine prescription group was low [2, 3, 5, 6, 8, 9]. The fact that most routine CXRs turned out to be futile was not surprising, since the presence of an important abnormality on the CXR, while no clinical change has been noticed, is very unlikely. Similarly, the probability that a routine CXR would prompt therapeutic intervention is low, as almost all major findings are clinically anticipated. These results were intuitive, but had not yet been clearly proven.
Some limits of our study need to be discussed. First, one may argue that routine CXRs are useful for checking the right position of invasive devices. In particular, the incidence of ETT malpositioning is high enough to warrant a systematic CXR after intubation [12]. This is why we did not include patients immediately after intubation. According to a nurses' protocol in use in our unit, once the ETT was rightly positioned, its length at the patient's lips was recorded, and nurses made sure it was still in place each time the patient was moved for whatever reason. Thus, no ETT malpositioning was observed during the study period. CXRs are also undoubtedly mandatory after central venous devices or NGT insertion. As they are mandatory, they cannot be considered routine (i. e., non-clinically indicated) CXRs. For this reason, they were not taken into account in the analyses. They were interpreted by junior physicians not involved in the study to avoid any potential bias. Second, one may also consider routine CXRs a reliable examination on which to base further, more specific diagnostic procedures (hemodynamic measurements or CT scan). For instance, the determination of the width of the vascular pedicle coupled with that of the cardiothoracic ratio could help assess the intravascular volume status [13, 14]. While this is not necessarily a reason to obtain daily films, it may add some value to CXRs in the ICU. Third, the attending physicians were not blinded to the assignment of patients. It may be argued that they paid more attention to clinically indicated CXRs, thus biasing the results toward higher diagnostic and therapeutic efficacy of the restrictive strategy. However, the fact that no difference between groups was observed when only clinically indicated CXRs of the routine prescription group were retained for analysis runs counter to this argument. Fourth, a radiologist did not interpret the CXRs. If this had been the case, the rate of new findings could have been higher. Nevertheless, it is doubtful that senior intensivists missed major diagnoses. Moreover, having CXRs interpreted by a radiologist would have implied modification of our usual practice. Fifth, some specific subgroups, such as patients with acute respiratory distress syndrome or immunodeficiency, may draw benefits from routine surveillance. No subgroup analyses were performed, however, owing to the small number of patients. Further studies are needed to evaluate this issue. Of note, CXRs are commonly difficult to interpret in those patients, and CT scanning may then be the procedure of choice [15]. Sixth, we did not specifically evaluate the potential reduction in costs or radiation exposure, but limiting the amount of CXRs would logically yield such secondary benefits. Finally, it must be emphasized that the value of routine CXRs will have to be reappraised when complete conversion from conventional film-based systems to digital chest image acquisition (which undoubtedly provides a substantial gain in diagnostic yield [16]) has been achieved.
In conclusion, we demonstrated that restrictive use of CXRs in mechanically ventilated patients in the ICU was associated with better diagnostic and therapeutic efficacy than systematic use, without impairing patients' outcome. Thus, our study lends support to protocols advocating clinically indicated rather than daily routine CXRs, at least until digital radiography is widely available.
References
Bekemeyer WB, Crapo RO, Calhoon S, Cannon CY, Clayton PD (1985) Efficacy of chest radiography in a respiratory intensive care unit. A prospective study. Chest 88:691–696
Brainsky A, Fletcher RH, Glick HA, Lanken PN, Williams SV, Kundel HL (1997) Routine portable chest radiographs in the medical intensive care unit: effects and costs. Crit Care Med 25:801–805
Hall JB, White SR, Karrison T (1991) Efficacy of daily routine chest radiographs in intubated, mechanically ventilated patients. Crit Care Med 19:689–693
Bhagwanjee S, Muckart DJ (1996) Routine daily chest radiography is not indicated for ventilated patients in a surgical ICU. Intensive Care Med 22:1335–1338
Chahine-Malus N, Stewart T, Lapinsky SE, Marras T, Dancey D, Leung R, Mehta S (2001) Utility of routine chest radiographs in a medical-surgical intensive care unit: a quality assurance survey. Crit Care 5:271–275
Fong Y, Whalen GF, Hariri RJ, Barie PS (1995) Utility of routine chest radiographs in the surgical intensive care unit. A prospective study. Arch Surg 130:764–768
Price MB, Grant MJ, Welkie K (1999) Financial impact of elimination of routine chest radiographs in a pediatric intensive care unit. Crit Care Med 27:1588–1593
Silverstein DS, Livingston DH, Elcavage J, Kovar L, Kelly KM (1993) The utility of routine daily chest radiography in the surgical intensive care unit. J Trauma 35:643–646
Graat ME, Choi G, Wolthuis EK, Korevaar JC, Spronk PE, Stoker J, Vroom MB, Schultz MJ (2006) The clinical value of daily routine chest radiographs in a mixed medical-surgical intensive care unit is low. Crit Care 10:R11
Greenbaum DM, Marschall KE (1982) The value of routine daily chest x-rays in intubated patients in the medical intensive care unit. Crit Care Med 10:29–30
Krivopal M, Shlobin OA, Schwartzstein RM (2003) Utility of daily routine portable chest radiographs in mechanically ventilated patients in the medical ICU. Chest 123:1607–1614
Brunel W, Coleman DL, Schwartz DE, Peper E, Cohen NH (1989) Assessment of routine chest roentgenograms and the physical examination to confirm endotracheal tube position. Chest 96:1043–1045
Ely EW, Haponik EF (2002) Using the chest radiograph to determine intravascular volume status: the role of vascular pedicle width. Chest 121:942–950
Ely EW, Smith AC, Chiles C, Aquino SL, Harle TS, Evans GW, Haponik EF (2001) Radiologic determination of intravascular volume status using portable, digital chest radiography: a prospective investigation in 100 patients. Crit Care Med 29:1502–1512
Schueller G, Matzek W, Kalhs P, Schaefer-Prokop C (2005) Pulmonary infections in the late period after allogeneic bone marrow transplantation: chest radiography versus computed tomography. Eur J Radiol 53:489–494
McAdams HP, Samei E, Dobbins J III, Tourassi GD, Ravin CE (2006) Recent advances in chest radiography. Radiology 241:663–683
Author information
Authors and Affiliations
Corresponding author
Additional information
Descriptor: Respiratory monitoring
Rights and permissions
About this article
Cite this article
Clec’h, C., Simon, P., Hamdi, A. et al. Are daily routine chest radiographs useful in critically ill, mechanically ventilated patients? A randomized study. Intensive Care Med 34, 264–270 (2008). https://doi.org/10.1007/s00134-007-0919-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0919-1